What do Restless Legs and Diabetes have in common? Other than that they both affect hundreds of millions of people, Restless Legs and Diabetes are commonly linked together. In this blog, we will cite excerpts from our peer-reviewed research, and dive into how these two diagnoses are connected, and reversed.
Very few are aware that Restless Legs is reversible. It’s important to understand that the treatment of both Restless Legs and Neuropathy is dominated by the pharmaceutical industry. Typically, doctors look to prescribe various medications as soon as you present symptoms. However, this blog will provide you with a non-medication approach. It all starts with doctors and patients having a better understanding of the peripheral nervous system, and its role in creating Neuropathy and Restless Legs symptoms.
The source of both Restless Legs Syndrome and Diabetic Neuropathy can both be the same.
Restless Legs Can Impact the Quality of Your Sleep and Life
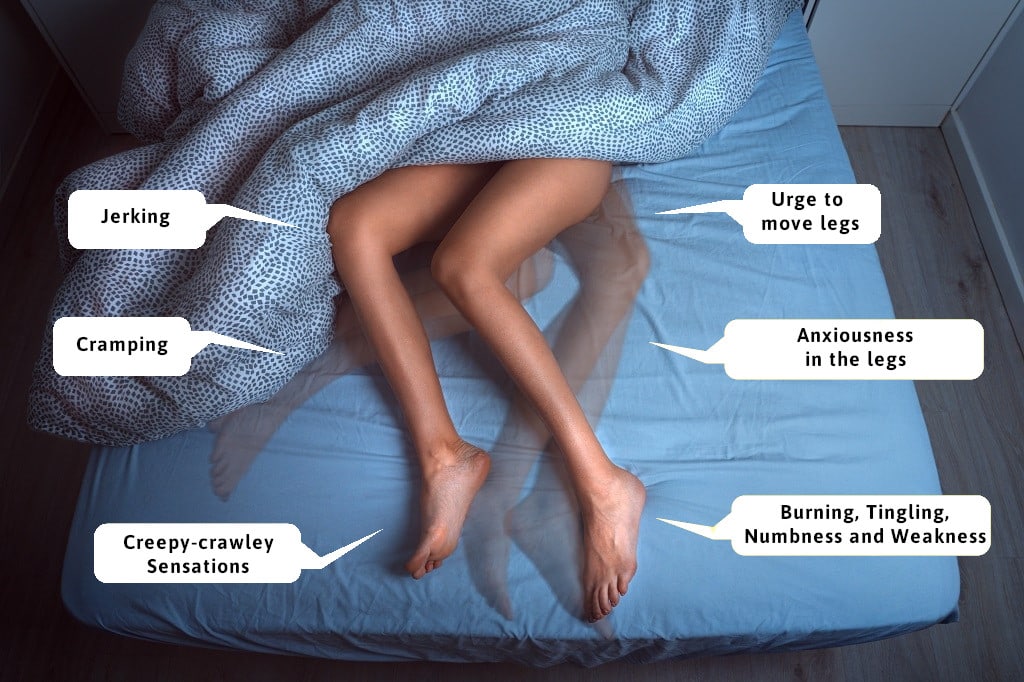
 Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.
Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.
Neuropathy Presents in 50 to 70 Percent of Patients With Diabetes
Symptoms of these patients include burning, tingling, numbness, and weakness. Conditions occur throughout the day and night, creating unhealthy sleeping patterns. There are two factors that make diabetics more likely to have neuropathy:
Polyol Pathway and Sorbitol
Sorbitol is a sugar that tends to reside in the nerve tissue of diabetics. Metabolically, when glucose levels are increased, glucose breaks down differently by the polyol pathway; and the by-product is sorbitol. When sorbitol gets into the nerve, more water is attracted to the nerve and the nerve enlarges. Studies have shown that diabetics may have a 40 percent increase in size. Since the nerves in the legs and feet travel through nerve tunnels (similar to carpal tunnel in the hands), the nerves become compressed and squeezed. This then causes nerve damage when blood sugars are high.
Malliard Effect
A French doctor by the name of Louis Malliard, first described this phenomenon. When you combine proteins that comprise our soft tissue structures, and glucose, you get advanced glycation end products (AGP). This causes the soft tissues to become more rigid, scarred, and less elastic. It leads to more damage to the diabetic nerve because the nerve tunnels that our nerves travel through, are now more rigid and can create high levels of compression on the nerves.
In summary, both the Polyol Pathway and the Malliard Effect increase the possibility of compression of nerve tunnels in the legs and feet. If this is new to you, do not fear. There is abbundant research to explain what the Maillard Effect and Polyol Pathway do to your body metabolically. In other words, it is crucial to look at biochemistry to see if medications may be helpful. Dr. James Anderson’s original research on Restless Legs, and a large volume of research on diabetic neuropathy, are leading down a different pathway. He likes to refer to it as the MECHANICAL PATHWAY. As you are beginning to understand these two processes, you can identify the negative effects on your nerves and body tissue. The net result of both is increased nerve compression in the nerve tunnels.
What Does the Research Say About the Connection Between Restless legs and Diabetic Neuropathy?
There are studies to support that if you have diabetes, the likelihood of you having Restless Legs increases. One study showed an increased chance of Restless Legs in patients with diabetes of 18-29 percent, compared to 6-7 percent in the control group. (1) Another study reports similar findings. (2) So as you can see, the odds of getting neuropathy as a diabetic are increased. Unfortunately, the same is true that if you have diabetes, you are more likely to have Restless Legs , which is secondary to diabetes.
What Our Research Shows to Support a Non-Drug Solution!
So, if we’re saying compression plays a role in diabetes being linked to neuropathy and Restless Legs , what evidence can we present to support this?
In relation to diabetic neuropathy, for almost two decades, Dr. Anderson has been decompressing nerve tunnels that become tight to reverse diabetic and non-diabetic neuropathy. Two of his peer-reviewed papers will show you that when we tested nerves intraoperatively using EMG testing, we could objectively demonstrate the improvement of nerve function in diabetics. For many, the improvement was well over 100 percent, and approaching 300 percent for some.(3)
In relation to Restless Legs, for the last 9 years, Dr. Anderson has taken charge to prove that for a majority of patients with severe Restless Legs, surgical decompression of nerve tunnels can provide a solution. You can also review the first peer-reviewed research paper on this concept.(4)
Conclusion: There Are More Pathways to Explore
So, from Dr. Anderson’s own personal experience as a peripheral nerve surgeon, he affirms that if you have diabetes, there is a greater chance that you will have neuropathy and Restless Legs. Research clearly shows there is a relationship between the two. The commonality is that both can be from compression, and diabetes increases the chances of having both.
The next question to answer is: Why do some patients with compression in their nerve tunnels get neuropathy symptoms, and others get Restless Legs symptoms? Although research on this is fairly limited, our team plans to share theories in some of our future blogs. For many of you, it is possible that you will persist in opting for conventional medicine. This has become a monetization approach for doctors which include Ropinirole, Mirapex, Neurontin, and other narcotics.
For many with minimal symptoms in early stages, the medications may be appropriate. However, for those with severe symptoms, the lack of quality of life and the possibility of severe mental and physical health issues might be compelling to consider other options. This “other option” suggests Restless Legs can be related to a mechanical compression issue. We always encourage our patients to be continuously engaged and educated on the subject. Dr. Anderson’s book, A Perfect Night’s Sleep, might help you make a connection between your diabetes and restlessness. Always remember, there is hope for you to have them reversed.
Dr. James Anderson
References:
- Mehdi Zobeiri, Azita Shokoohi, “Restless Leg Syndrome in Diabetics Compared with Normal Controls”, Sleep Disorders, vol. 2014, Article ID 871751, 4 pages, 2014. https://doi.org/10.1155/2014/871751
- Giovanni Merlino, MD, Lara Fratticci, MD, Mariarosaria Valente, MD, Angela Del Giudice, MD, Claudio Noacco, MD, Pierluigi Dolso, MD, Iacopo Cancelli, MD, Anna Scalise, MD, PhD, Gian Luigi Gigli, MD, Association of Restless Legs Syndrome in Type 2 Diabetes: A Case-Control Study, Sleep, Volume 30, Issue 7, July 2007, Pages 866–871, https://doi.org/10.1093/sleep/30.7.866
- https://andersonpodiatrycenter.com/dr-anderson-sharing-his-research-and-expertise-internationally/
- James C. Anderson, Megan L. Fritz, John-Michael Benson, Brian L. Tracy, Nerve Decompression and Restless Legs Syndrome: A Retrospective Analysis, Front. Neurol., 06 July 2017, https://www.frontiersin.org/articles/10.3389/fneur.2017.00287
https://andersonpodiatrycenter.com/dr-anderson-sharing-his-research-and-expertise-internationally/