 Opiate Addiction
Opiate Addiction
Chronic nerve pain is a very common problem and maybe dangerous because of the overuse of narcotics and the potential for opioid addiction. And as you may have heard in the news approximately 80,000 – 90,000 people have died from drug overdoses annually in recent years. Chronic pain is becoming a big health crisis in this country. The purpose of this blog is to help you challenge what you’ve been told about chronic nerve pain and look at a new approach that gives you hope for a permanent solution.
First, what is nerve pain?
Nerve pain is commonly referred to as neuropathic pain. The symptoms of neuropathic pain include burning, tingling, numbness, and sharp stabbing pain. These nerve pain symptoms may make activities difficult because of pain or lack of balance from numbness. Numbness can cause an additional risk as the pain signals that normally go to the brain from the foot may not warn of a sore or injury because of damage to the nerves. For many, sleeping may be difficult as even sheets touching your skin may be painful. The nervous system can be divided into two areas. The central nervous system includes the brain and spinal cord and the peripheral nervous system which includes nerves traveling into the arms and legs. When talking about neuropathic pain, we’re referring to pain in the peripheral nervous system. In the lower extremity, this includes the nerves that extend from the spinal cord down into the legs and feet. Nerve pain can be from various causes. Neuropathy is one of the most common. Neuropathy can be caused by diabetes {diabetic neuropathy}, from unknown causes{idiopathic neuropathy }, or related to other causes such as alcoholism, toxins, chemotherapy, and autoimmune disease. Chronic nerve pain may also be caused by injuries such as a fracture, a severe sprain, or even surgery. This is commonly referred to as regional pain syndrome. But the symptoms for all of these can be very similar in terms of how they present.
The conventional approach
The medical advice many patients are hearing can be divided into two categories.
Live with your pain or take drugs – For many, the pain treatment includes taking pain medications such as Lyrica or Gabapentin. In severe cases, narcotics may be recommended. These medications may help with the symptoms but do nothing to get at the cause. Many patients are told they have no other choice. So, whether it’s called neuropathy or chronic regional pain the treatments may be similar. Lyrica and Gabapentin have side effects that include weight gain and narcotics have the risk of addiction or overdose. So, the options you’ll hear are to live with it or take the medication.
Treat your back to help the symptoms in your feet and legs – Other patients are told that the neuropathic pain is from the back. Treatments are then offered that may include chiropractic treatment, physical therapy, or injections in the back. For others, it may even include back surgery or placing a nerve stimulator in the back. Again, the healthcare community including neurosurgeons, orthopedic surgeons, chiropractors, physical therapists are all trained to look at the back. Very few are well trained in the evaluation of the peripheral nervous system in the lower extremity.
So, if it’s not metabolic and treated with medication or it’s not from the back and treatment is focused on the wrong source what’s another option?
The peripheral nervous system!
How do we treat neuropathic pain?
Treating the root cause of a problem, avoiding opioid addiction
The conventional medicine approach I just described could be considered as blowing on the smoke but not putting out the fire of nerve pain. As a peripheral nerve surgeon, I deal with patients that have chronic pain and various types of neuropathies and for many patients, the problem isn’t what we used to think it was. For some chronic pain can be from damage to nerves from trauma or from surgery. The pain from these nerves can be blocked by the removal of the damaged nerve branch in many cases. Surgery on the back, nerve stimulators in the back, and injections in the back can be avoided. This approach offers a better chance for permanent resolution. In the case of neuropathy, whether it’s diabetic or non-diabetic, it could be from tunnels that have become tight.
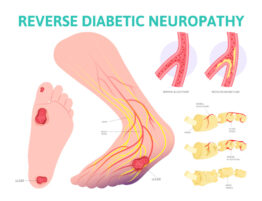
Research to support that diabetic neuropathy is reversible
We now know that the diabetic nerve will swell because of a sugar molecule that resides in the nerve tissues attracting water to the nerve. Because the nerve is swollen, it will now be subject to more pressure when it passes through nerve tunnel such a s the carpal tunnel in the hand. One study has shown this change of dimension in the similar tunnel in the foot, the tarsal tunnel. [1] The research that I’ve done includes two studies that give objective evidence with EMG testing of the diabetic nerves before and after the nerve tunnels are opened in surgery that the nerves are now functioning better. Larger impulses from the stimulated nerve go into the muscles that the nerve supplies after surgery compared to before the tunnel was opened. For many, there is at least an 80 chance of reversal of diabetic neuropathy symptoms. [2] [3]
There are other studies to support this concept. [4] [5] [6] Therefore the neuropathy you’ve been suffering from may be from compression in multiple nerve tunnels in the lower extremity much like the carpal tunnel in the hand.
So, if you’ve been told that it’s irreversible because it’s metabolic this may not be true. Yes, diabetes does affect the health of the nerves as do other metabolic problems, but there can also be an issue with nerve compression in tight nerve tunnels that is the cause. Why haven’t you heard this? This information is being drowned out by marketing. As an example, $272 million dollars were spent in 2018 to market one drug alone, Lyrica. [7]
The new way of looking at Chronic nerve pain- A solution to opioid addiction
Because of this new approach, many are looking for a peripheral nerve surgeon as another option. The treatments may include other non-surgical treatments. However, the focus of the treatment is to deal with the area of compression or nerve injury and by doing so, we are much more likely to have a long-lasting and possibly permanent effect on the patient’s chronic pain. This is important to know because the opioid crisis is almost at an epidemic proportion.
This information should challenge what you’ve been told about your chronic nerve pain. Hopefully, you’ll look deeper at this novel approach and judge for yourself. Armed with this information maybe you or someone you know can be saved from the potential risk of medicating your nerve pain. If you’ve been hiding in the bushes waiting for another option, please give us a call.
References
[1] Dauphinee
https://www.aens.us/images/aens/Lee-Dauphinee-2005.pdf
[2] Anderson
https://andersonpodiatrycenter.com/wp-content/uploads/2019/03/NIM-Study-published-copy.pdf
[3] Anderson
https://ur.booksc.eu/book/82143501/aa3266
[4] Zhang
https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0032-1320029
[6] Dellon
https://pubmed.ncbi.nlm.nih.gov/15566708/

 Opiate Addiction
Opiate Addiction



Write a comment: