Heel pain is one of the most common complaints that foot specialists encounter. Many people assume that pain in the bottom of the heel is caused by plantar fasciitis, which is true for most patients. However, another less common issue, known as heel pad syndrome, can also cause heel pain. In this blog, we will discuss the causes and treatment of heel fat pad syndrome. Additionally, you may have received a misdiagnosis, and we will explore a little-known condition that could explain why your treatments have not been successful.
The Basics: Heel Anatomy
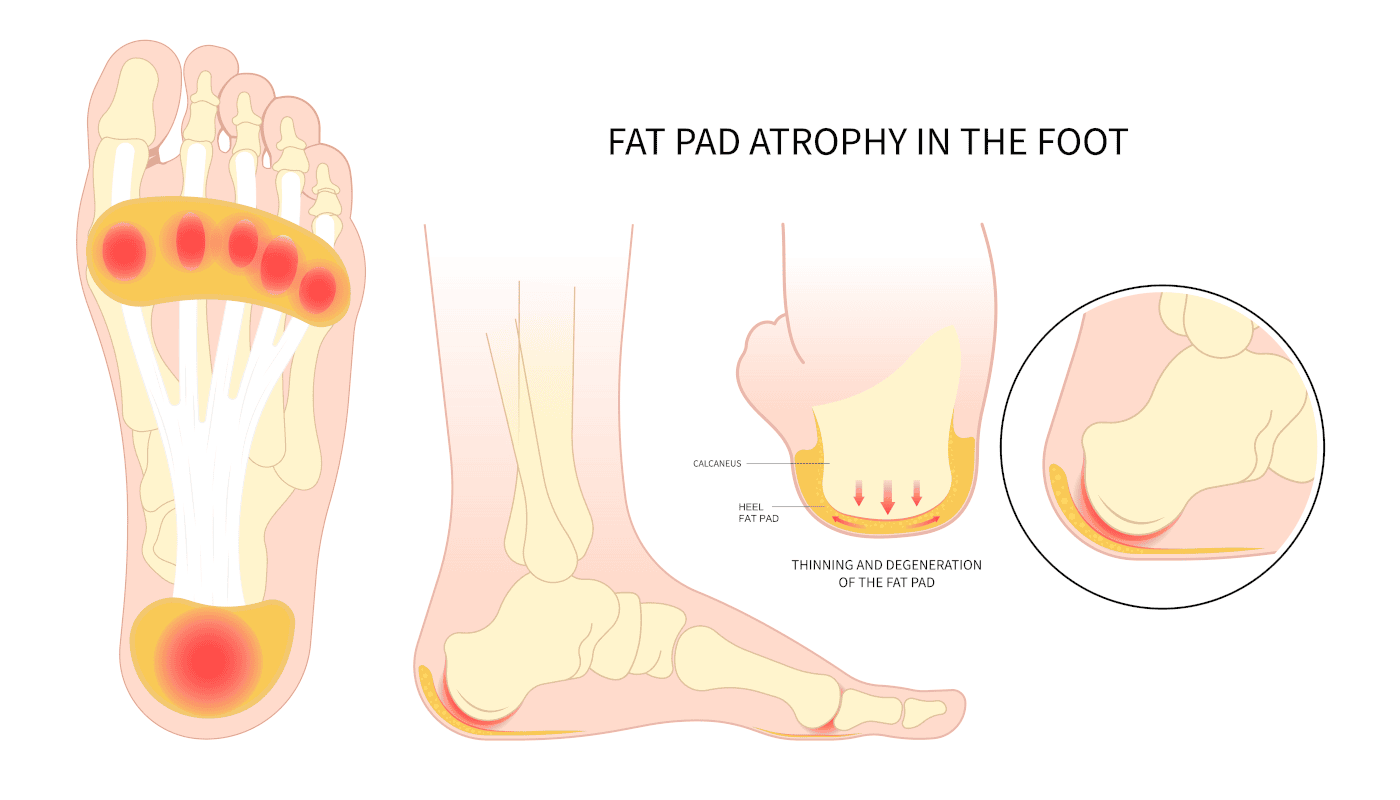
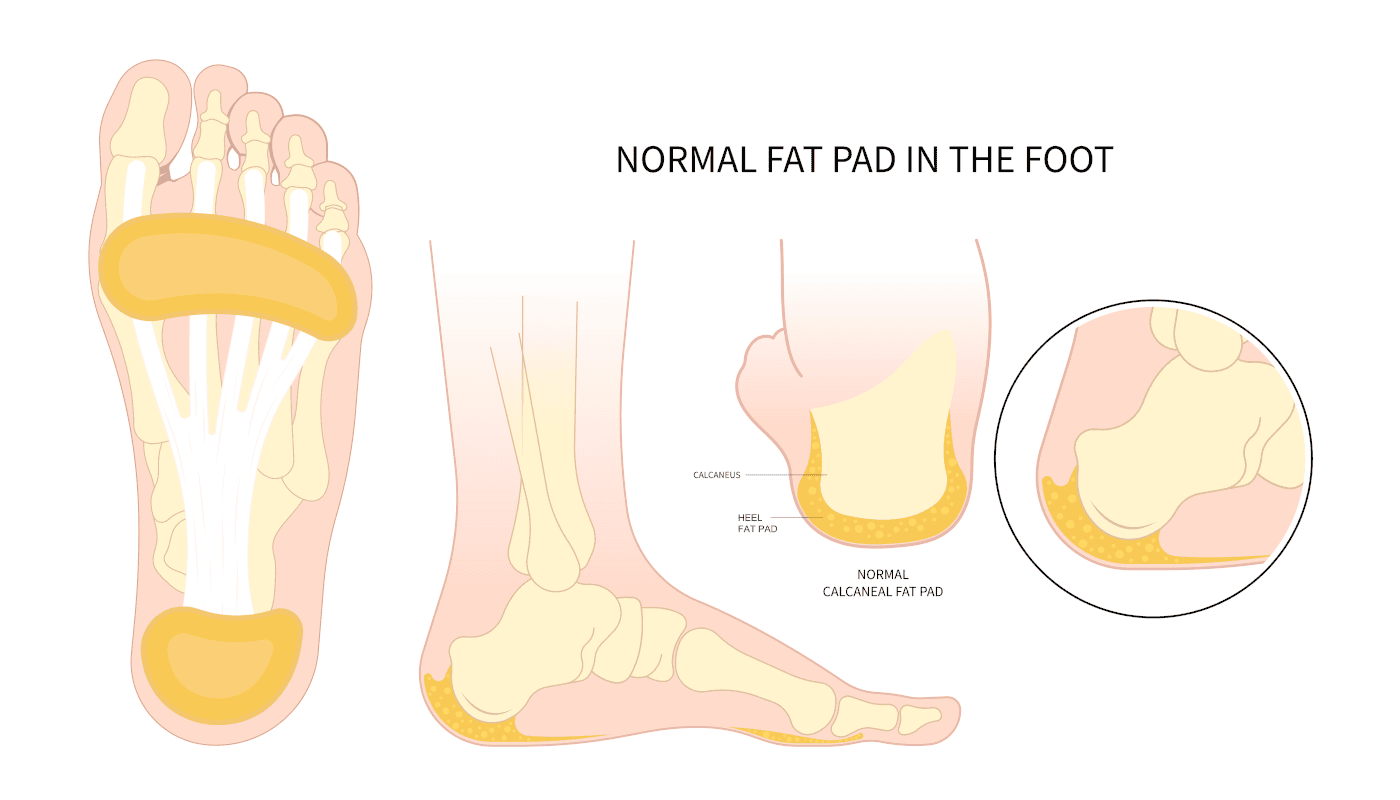
The foot is uniquely designed to absorb shock. As we walk or run, the foot strikes the ground with 3-4 times our body weight. To compensate for this, the heel, the softest bone in our body, dissipates that shock. Beneath the skin, a significant amount of fatty tissue is distributed throughout the bottom of the foot, providing additional cushioning.
Within the fat are tight connective tissues that act as a net to support the fat pad’s structure. On the bottom of the heel, x-rays may reveal a heel spur. Using ultrasound technology, a podiatrist can also detect abnormalities in the plantar fascia.
The plantar fascia originates in the ball of the foot, extends through the arch, and inserts at the bottom of the heel. With every step, the arch flattens, causing the fascia (a tight connective tissue) to pull on the heel.
Symptoms of Heel Pad Syndrome
When one is suffering from heel pad syndrome, the pain will be directly underneath the heel bone. Pain may be present first thing when you get up in the morning or when you walk throughout the day. The pain will not extend to the arch but is centered directly underneath the heel.
Causes of Heel Pad Syndrome
- Heredity – Some people may inherit a thinner fat pad from their parents.
- Cortisone Injections – Cortisone injections, which doctors may use to treat plantar fasciitis, can lead to heel pad syndrome and contribute to fat pad atrophy.
- Hard Surfaces – Walking or running barefoot, as well as engaging in activities on hard surfaces like concrete or wooden floors, can cause the fat pad to thin.
- Biomechanics – Certain foot structures are more likely to cause fat pad atrophy.
- Excess Body Weight – People who carry more body weight may increase their risk of developing heel pain. The added weight stresses and displaces the fat pad.
- Age – As we age, the fat pad naturally thins as part of the aging process.
- Metabolic Problems – Medical conditions like type 2 diabetes, lupus, and rheumatoid arthritis can increase the risk of developing heel pain.
Diagnosis of Heel Pad Syndrome:
- Symptoms – The doctor asks you about your symptoms, where they are located, and when they occur.
- Examination – The doctor examines your foot to determine where the pain is located.
- Testing – The doctor may take X-rays to rule out any bony involvement.
- Diagnostic Ultrasound – The doctor uses ultrasound to measure the thickness of the fat pad and evaluate the plantar fascial tissue in the affected area.
- MRI Imaging – The doctor may order an MRI to assess the fascia and fat pad, and more importantly, to rule out a stress fracture in the heel.
Treatments may include the following:
- Shoe Gear – Wearing shoes with extra cushioning can help provide relief.
- Heel Cups – It will help center the fat directly beneath the heel, preventing displacement from the middle when you bear weight.
- Medication – Taking anti-inflammatory medications can help reduce pain and inflammation.
- Icing – Applying ice can alleviate symptoms in mild cases of heel pad syndrome.
- Shoe Inserts – Using over-the-counter arch supports or custom-made orthotics can offer additional support and comfort.
Life style Changes:
- Avoid High-Impact Activities – Avoid high-impact activities like basketball that cause heel pain. Jumping and landing on your feet wear down the fat pad. Instead, opt for low-impact activities that involve softer surfaces like swimming.
- Maintain a Healthy Weight – Keeping a healthy weight reduces the impact and force on your feet, allowing for better distribution and control.
Why the diagnosis of Heel Pad Syndrome should throw up a red flag in your mind?
- Plantar Fasciitis – When it comes to pain in the bottom of the heel, the most common diagnosis is plantar fasciitis. To accurately diagnose this foot problem, patients with heel pain should undergo a diagnostic ultrasound. Using an ultrasound, a podiatrist can evaluate both the appearance and thickness of the fascia to confirm the diagnosis. Without this test, a definitive diagnosis cannot be made.
- Heel Spur – Heel spur pain is a common misconception. In the past, people believed that if a heel spur appeared on an x-ray, it was the source of pain. However, with the introduction of endoscopic surgery in the late 90s, this belief has become outdated. This advanced technique, which has proven highly successful in eliminating heel pain, changed the understanding of heel spur pain.
During this procedure, surgeons make small incisions on both sides of the heel, allowing them to visualize and cut a portion of the fascia to relieve tension. Interestingly, the success of this technique does not involve removing heel spurs, even though many patients undergoing the procedure have heel spurs. As a result, the idea that heel spurs cause pain has been invalidated. In fact, as early as the 1930s, medical literature stated that heel spurs develop due to the fascia pulling away from the heel, but the spur itself does not cause pain.
Your Fat Pad Syndrome Pain may truly be Nerve Pain. Are you misdiagnosed? Your Fat Pad Syndrome may be Nerve Pain.
The Medial Calcaneal Nerve Branch
The medial calcaneal nerve branch passes beneath the heel bone, located precisely where the pain occurs. This nerve originates from the posterior tibial nerve, which travels along the inside of your ankle. The posterior tibial nerve has branches that supply sensation to the bottom of the foot, much like the carpal tunnel area in the hand. Specifically, two branches in the tarsal tunnel extend to the arch and ball of the foot, providing sensation to these areas.
Meanwhile, the third branch, the medial calcaneal nerve, travels down the inside of your heel and supplies sensation to the bottom of the heel bone. On its way to the heel, it passes through a small tunnel on the inner side of the heel bone. This tunnel, composed of tightly connected tissue, can entrap or compress the nerve. Additionally, when the plantar fascia thickens in patients with plantar fasciitis, this nerve often becomes irritated. As a result, a patient may experience both plantar fasciitis and nerve pain simultaneously.
Diagnosis of Medial Calcaneal Nerve Branch Pain
-
-
- Clinically – The doctor evaluates the heel by checking for discomfort, which usually occurs on the inner side of the heel bone.
- Diagnostic Injections – The doctor may administer an injection at the entrapment site of the nerve. The location is on the inside of the heel and then it follows beneath the heel bone. When patients respond favorably with a significant reduction in pain, this confirms the diagnosis.
-
Treatment
-
-
- Cortisone Injections – Doctors can use cortisone injections to help confirm the diagnosis, and a series of two or three injections can eliminate the pain.
- Radio Frequency Nerve Ablation Technique – This technique effectively blocks the pain signals in the nerve.
- Surgery – As a last resort, surgeons can resect the nerve and bury it into the muscle in the lower leg.
-
Have you been told you have heel pad syndrome and the attempts by your doctor have failed? Please consider the little-known diagnosis of medical calcaneal nerve branch entrapment. This may truly be what is slowing you down and causing your heel pain. This is why you should contact our certified foot doctors.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.